Team Viz
Jul 24, 2025
By Tom Krohn, Global Pharma Commercial Lead, Viz.ai
Let’s be honest: the number of tech failures in healthcare is staggering. And it’s not because the software crashed or the algorithm was wrong. It’s because we keep missing the real problem.
For all the talk of transformation, most digital health solutions land with a thud. According to Gartner, up to 85% of digital health initiatives fail to deliver sustainable impact. Billions are spent, pilots are run, press releases are issued—and yet care delivery remains largely the same, only now with more screens and administrative clicks.
This isn’t a technology failure. It’s a failure of alignment.
We continue to throw tech at problems without deeply understanding the environment it’s being dropped into. In healthcare, that’s a guaranteed way to fail.
Tech Alone Doesn’t Save Us
Let’s rewind to the rise of Electronic Health Records (EHRs). Technologically, they were a success: they digitized records across the industry. But in practice, they often burden clinicians with complex workflows and documentation overhead. Why? Because they weren’t designed to serve the clinician’s needs—they were built to support billing and regulatory compliance.
This is the pattern: innovation that doesn’t align with real-world clinical and operational needs dies, regardless of how sophisticated the technology is.
As Clayton Christensen reminded us in The Innovator’s Prescription, the true disruptive force in healthcare isn’t tech alone—it’s a shift in business models that better address the job to be done.
Why Most Innovation Never Crosses the Chasm
Geoffrey Moore’s Crossing the Chasm taught us that early adopters may get excited by new technology, but mainstream users require workflow integration, trust, and clear value. That’s a steep climb in healthcare, where systems are complex, incentives are misaligned, and clinical teams are already stretched thin.
IBM Watson’s AI for cancer care failed not because it wasn’t cutting-edge, but because it didn’t mesh with how oncologists actually work. It didn’t add value at the point of care. It added friction.
It’s not that we lack brilliant engineers. We lack solutions built with—and for—the people who deliver care.
When the Stars Align
When innovation works in healthcare, it’s not because of the tech alone—it’s because all the stakeholders are considered, aligned, and equipped.
Teladoc Health didn’t invent video visits. But it thrived because it aligned with patient convenience, payer reimbursement models, and provider flexibility. It solved a real coordination problem across the value chain.
And I’ve seen this firsthand at Viz.ai, where I work.
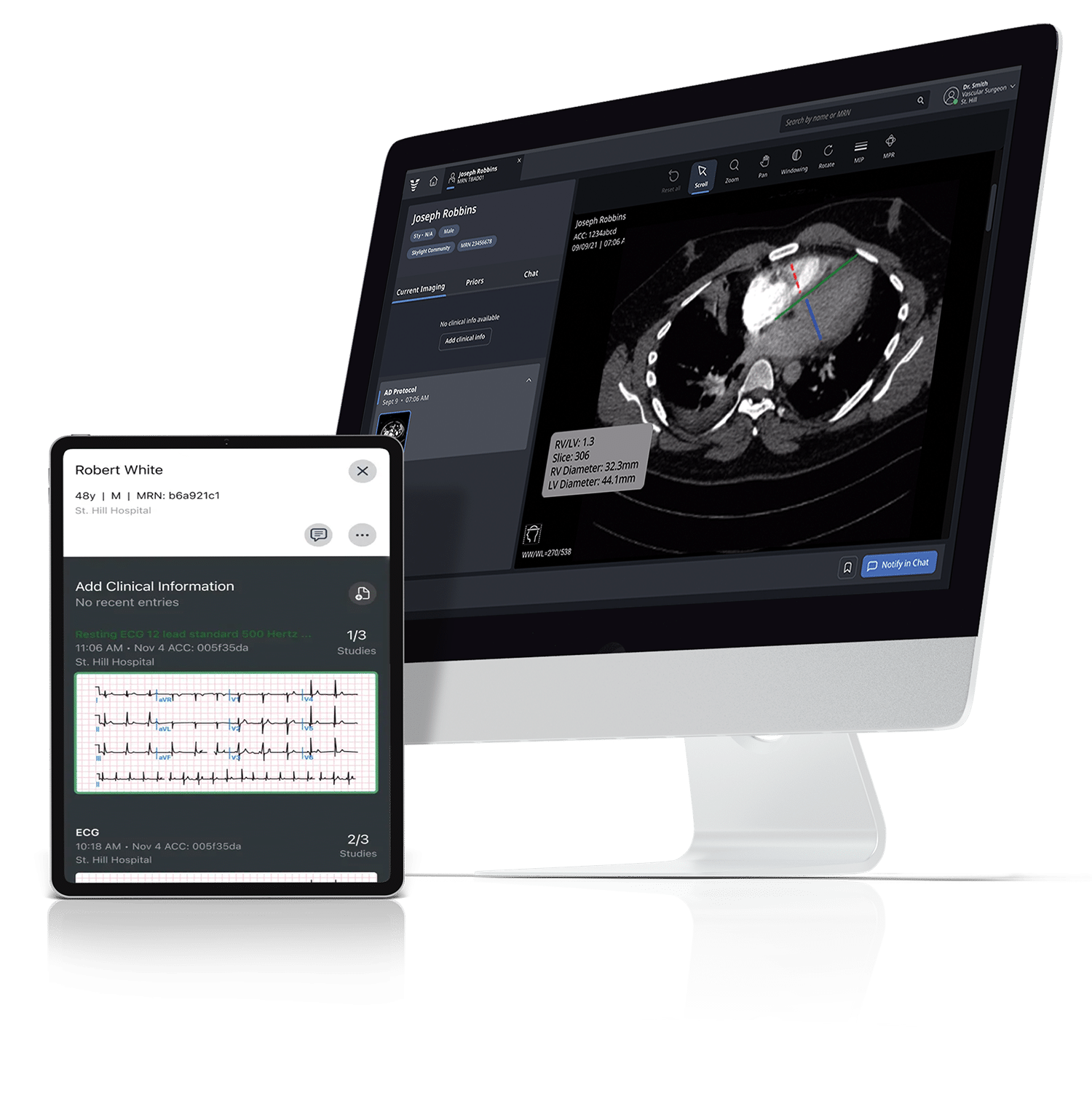
One of our neuro products at Viz.ai uses AI to detect early signs of stroke and immediately mobilize the care team—radiologists, neurologists, neuro-interventionists, ED staff—all in sync and in real time. It’s not just AI for the sake of AI. It’s AI plus care coordination, designed to compress time, reduce variability, and improve outcomes.
Our stroke platform was the first AI software granted FDA clearance via the de novo pathway. But that was just the beginning. We’ve since expanded across the country and influenced American Heart Association guidelines—proof not just of innovation, but of adoption and impact.
Why has Viz.ai succeeded where so many others have failed? Because we build with the job to be done in mind. Because we understand that it’s not enough to detect a problem—you need to activate the system to solve it. That’s the difference.
A recent article in Nature highlighted the holistic approach of what it takes for successful commercialization of medical AI. A good reminder and review of key components, though I think they missed the hard part. The human side of behavioral change.
What Now? The Hard, Uncomfortable Truth
Here’s the part no one wants to hear: this work is hard. There is no silver bullet.
Creating lasting change in healthcare means doing the deep work—understanding every stakeholder’s incentives, mapping operational realities, and embedding change into systems that resist it.
While there are clear frameworks such as AIM for change management, it takes time, resources, patience, and persistence. It requires talking to clinicians, sitting in on workflows, shadowing case managers, and understanding CFO dashboards. It demands we build solutions that are trusted, not just tested. Solutions that fundamentally help the system improve its care and align to incentives and motivations to show demonstrated value over time.
And yes, that means sometimes we say “no” to building something cool if it won’t work in the real world.
So, Where Do You Begin?
Start here:
- Ask what the job is—not just for the clinician, but for the administrator, the patient, and the system as a whole.
- Follow the incentives. If the payment model punishes your innovation, you’re already in trouble.
- Design for trust and ease of use. Especially in healthcare, if it doesn’t feel safe or seamless, it won’t scale.
- Test in context. Not in a lab, but in a hospital hallway, at point of care and decision making, or a nurse navigator’s review list.
That’s where real innovation lives.
⸻
Let’s Talk
I’ve spent 35 years working on both the failures and successes of healthcare innovation. If you’re tired of launching tech that doesn’t stick—or want to build something that truly changes care—let’s connect.
I’d love to help you solve for the root, not just the symptoms. Reach out here or at tom.krohn@viz.ai.