Team Viz
Aug 14, 2025
By Bill Stadtlander, VP of Life Sciences Commercial, Viz.ai
Despite the trillions of dollars funneled into the U.S. healthcare system, our outcomes tell a different story. Healthcare now accounts for over 17% of our GDP1, yet we consistently fall behind on critical health metrics. Too many patients remain undiagnosed, underserved, or stuck in care silos—often because the system simply can’t keep up.
We face a fundamental access problem: access to timely diagnosis, to specialists, to guideline-directed therapies, and even to basic care coordination. The cracks in the system aren’t just inefficiencies, they’re lost lives, delayed treatments, and missed opportunities for better outcomes.
Artificial Intelligence (AI) offers a way to bridge those gaps, creating faster, smarter, and more equitable care pathways that improve patient access from the very first signal of disease to long-term management.
The Problem: Fragmented Pathways and Delayed Care
One of the greatest challenges in healthcare today is the variability in how patients move—or fail to move—through the system. Diagnostic delays, uneven provider knowledge, and inconsistent adherence to guidelines all play a role. Many diseases, particularly rare or complex ones, take years to diagnose. Others are caught late when symptoms finally become severe.
On the provider side, burnout has reached record levels. HCPs are expected to manage more patients with less time, less support, and more administrative burden. This human cost creates a bottleneck for patient access, particularly in resource-limited or high-volume settings.
AI as a Bridge, Not a Band-Aid
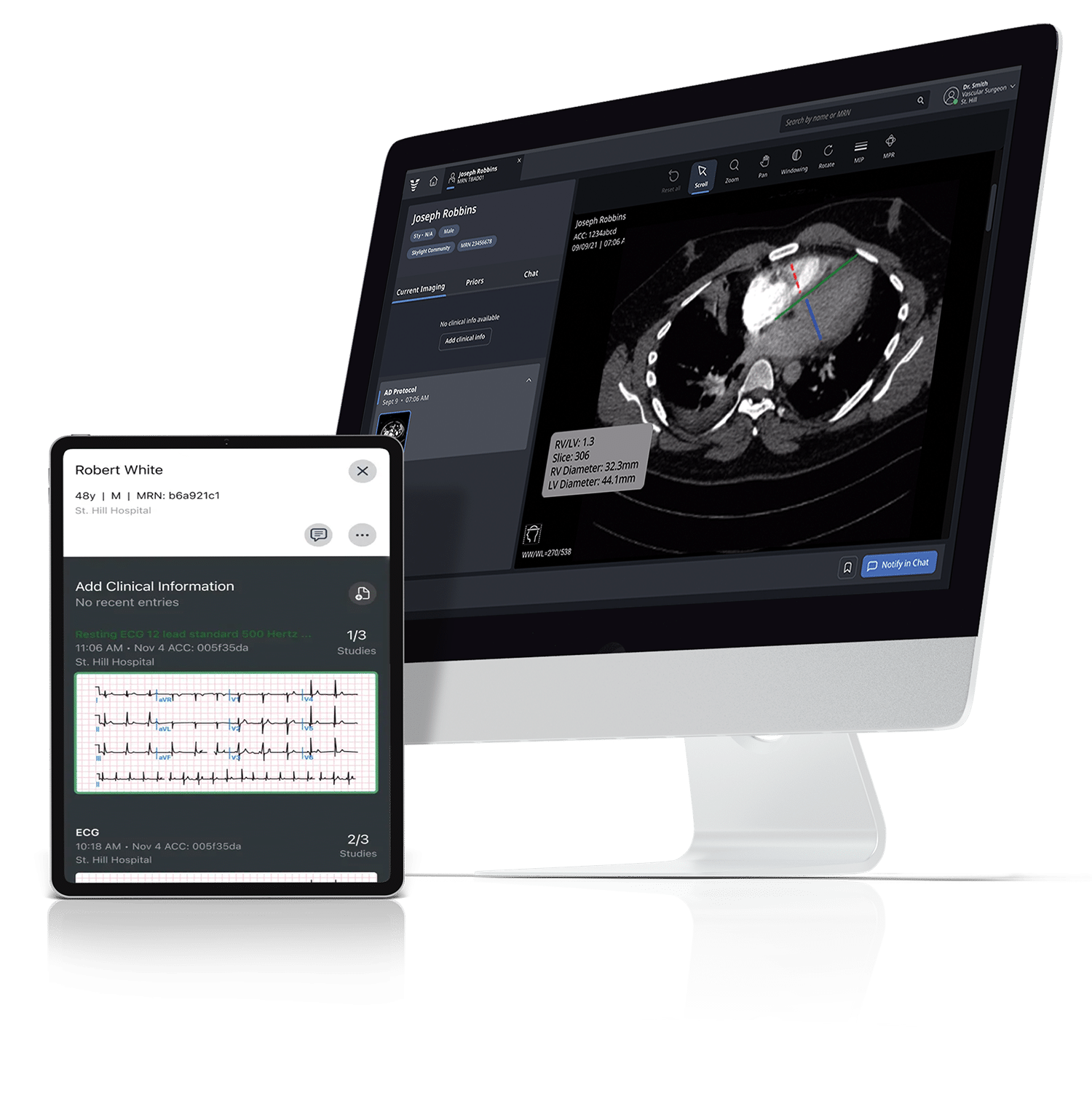
AI can help reshape this broken equation—not by replacing HCPs, but by supporting them. By embedding AI into care pathways, we can proactively surface high-risk patients, standardize diagnosis, and accelerate time to treatment.
We see AI’s impact in two primary categories:
1. Automating What Humans Already Do
Many AI tools today focus on tasks HCPs perform manually—just much faster. Our Viz stroke solution (Viz LVO™), for example, automatically analyzes MRI and CT scans to detect large vessel occlusions (LVOs) or hemorrhagic strokes. Rather than waiting for radiology to flag a scan, our solution can alert the care team in real time—cutting time to treatment by over 60 minutes. In stroke care, that translates to 120 million brain cells saved per patient.
This kind of automation improves access by reducing delays and enabling rapid triage, especially in under-resourced hospitals where time and expertise are in short supply.
2. Providing Super Human Powers
More transformative still are AI tools that go beyond what humans can reasonably detect. Our Viz Hypertrophic Cardiomyopathy (HCM) algorithm (Viz HCM™), for example, uses ECG data to identify signs of HCM—a condition that takes an average of five years to diagnose. We’re currently screening millions of ECGs using a de novo ECG-based model to screen for HCM reducing diagnosis to just three months.
These innovations allow us to reach more patients earlier, especially those who may otherwise be missed due to lack of symptoms or access to specialty care.
The Care Pathway of the Future
To deliver true value, AI must be more than a feature—it must be integrated across the patient care journey:
- Detection: AI-powered tools identify subtle indicators of disease from imaging, labs, ECGs, or even unstructured notes.
- Triage: Patients are prioritized based on urgency and risk assessing, enabling more efficient use of limited specialist resources.
- Care Coordination: Automated workflows streamline communication, referrals, and follow-ups, reducing drop-off and delay.
- Decision Support: AI copilots assist providers at the point of care, offering intelligent disease specific summaries and evidence-based suggestions integrated into the EHR.
Partnering to Expand Access at Scale
One of the most exciting developments in our mission to improve patient access is the momentum behind our partnerships with life sciences companies. Viz.ai has teamed up with 11 leading biopharma and medtech innovators including Bristol Myers Squibb, Novartis, Sanofi, and Regeneron to develop AI-powered workflows that better support HCP and patient journeys..
These collaborations are grounded in a shared commitment to advancing patient care by enabling earlier detection, faster diagnosis, and more equitable access for all patients to guideline-directed therapies. Together, we are addressing a wide range of life-threatening and debilitating conditions — from oncology, to chronic diseases such as COPD, and cardiovascular conditions ranging from common to rare. By developing and deploying holistic care pathway solutions we are getting the right patient to the right specialist to the right treatment, faster.
Why AI Adoption Still Lags
Despite its potential, AI adoption in healthcare still faces significant headwinds:
- Data Access: Many AI solutions need high-quality clinical data, which is often siloed within EMRs or difficult to extract at scale.
- Workflow Fit: Providers don’t want 20 different apps—they want seamless, in-workflow solutions that work the way they work.
- Trust & Transparency: HCPs need to understand why an AI model made a recommendation, not just what it concluded.
- Regulatory & Reimbursement Barriers: A lack of FDA clarity or CPT codes for AI-enabled services limits scalability.
- Risk Aversion: “First do no harm” is a sacred principle. AI must prove itself safe, reliable, and additive to care—not experimental.
At Viz.ai, we address these head-on through a hybrid model. We use general-purpose LLMs tools for language generation and build custom, domain-specific models for clinical precision. Every step is anchored in transparency, piloting, and trust-building—with HCPs always in the driver’s seat.
Closing the Loop on Access
Bridging the access gap isn’t just about diagnosing faster—it’s about ensuring that no patient gets lost along the way. AI can guide patients from first signal to diagnosis, to treatment—efficiently, equitably, and at scale.
Our work with health systems and life sciences partners proves that scalable, AI-powered pathways aren’t just possible—they’re already here. The future of healthcare depends not just on what we build, but how we connect it. AI, when deployed with thoughtfulness and purpose, is the bridge we need to close the care gap once and for all.
1 Centers for Medicare & Medicaid Services (CMS). National Health Expenditure Data: Historical. Updated December 13, 2023. Accessed August 13, 2025. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical