Team Viz
May 28, 2025
Written by David Z. Rose, MD, Professor, Vascular Neurology, University of South Florida Morsani College of Medicine
The Many Faces of Cryptogenic Stroke
For patients with cryptogenic stroke, the cause may for a long time remain labelled “cryptic” – a hidden source with an unknown risk of subsequent stroke.1 However, a team with a thorough and cohesive plan may uncover the etiology in order to prevent the next stroke. This can only be accomplished with well-designed, evidence-based, patient-specific workflows, appropriate intervention and tailored therapy. Over the past decade, the increasing use of cardiac monitoring has led to increased detection of paroxysmal Atrial Fibrillation (AFib), an arrhythmia which appears and disappears. The value of finding AFib is that superior therapeutic decisions can be made by providers: instead of prescribing simply an aspirin a day for cryptogenic stroke, patients who are found to have AFib can be more appropriately treated with anticoagulation (AC) or left atrial appendage closure (LAAC).
The new artificial intelligence (AI)-powered care coordination platform designed by Viz.ai, called Viz Connect®, addresses this issue by connecting neurology and cardiology teams directly for cardiac evaluation prior to hospital discharge. This approach has been shown to improve patient outcomes and offer operational and economic benefits to healthcare systems.
Guidelines state that patients with cryptogenic stroke should receive Cardiology evaluation, however, significant heterogeneity in post-stroke cardiac monitoring exists. In the 2024 DiVERT-Stroke study2 community hospitals reported 2.5-times more cryptogenic stroke than academic centers, yet ordered 10-times fewer short/long-term cardiac monitors to look for AFib. Efforts to reduce heterogeneity are warranted to improve AFib detection and then offer best treatment to prevent stroke recurrence.2
To resolve that issue, the Viz.ai care pathway for cryptogenic stroke, Viz Connect®, extends the neurology workflow into the cardiology department. Viz Connect serves as a checkpoint reminder for providers caring for cryptogenic stroke patients to order potentially life-saving cardiology consultation so those patients can get monitored for AFib.
AI-Powered Care Coordination
Today, almost every stroke center in the United States uses AI to help detect and triage stroke faster. Use of AI software was incorporated into the clinical guidelines by the American Heart Association in 2023 as standard of care. The Viz LVO® (large vessel occlusion) module, for example, detects a suspected stroke in real-time by computed tomography angiography (CTA). Then, it auto-alerts the on-call stroke team with HIPAA-compliant communication tools.
Traditionally, patients are advised to follow up with a cardiologist after discharge for further evaluation. While a consult may occasionally be placed through the EMR, it may take days for cardiology to receive and act upon it, by which time the patient has already left the hospital. Without timely communication or a clear sense of urgency, many patients fail to follow through, missing critical evaluations that could reduce their risk of another stroke.
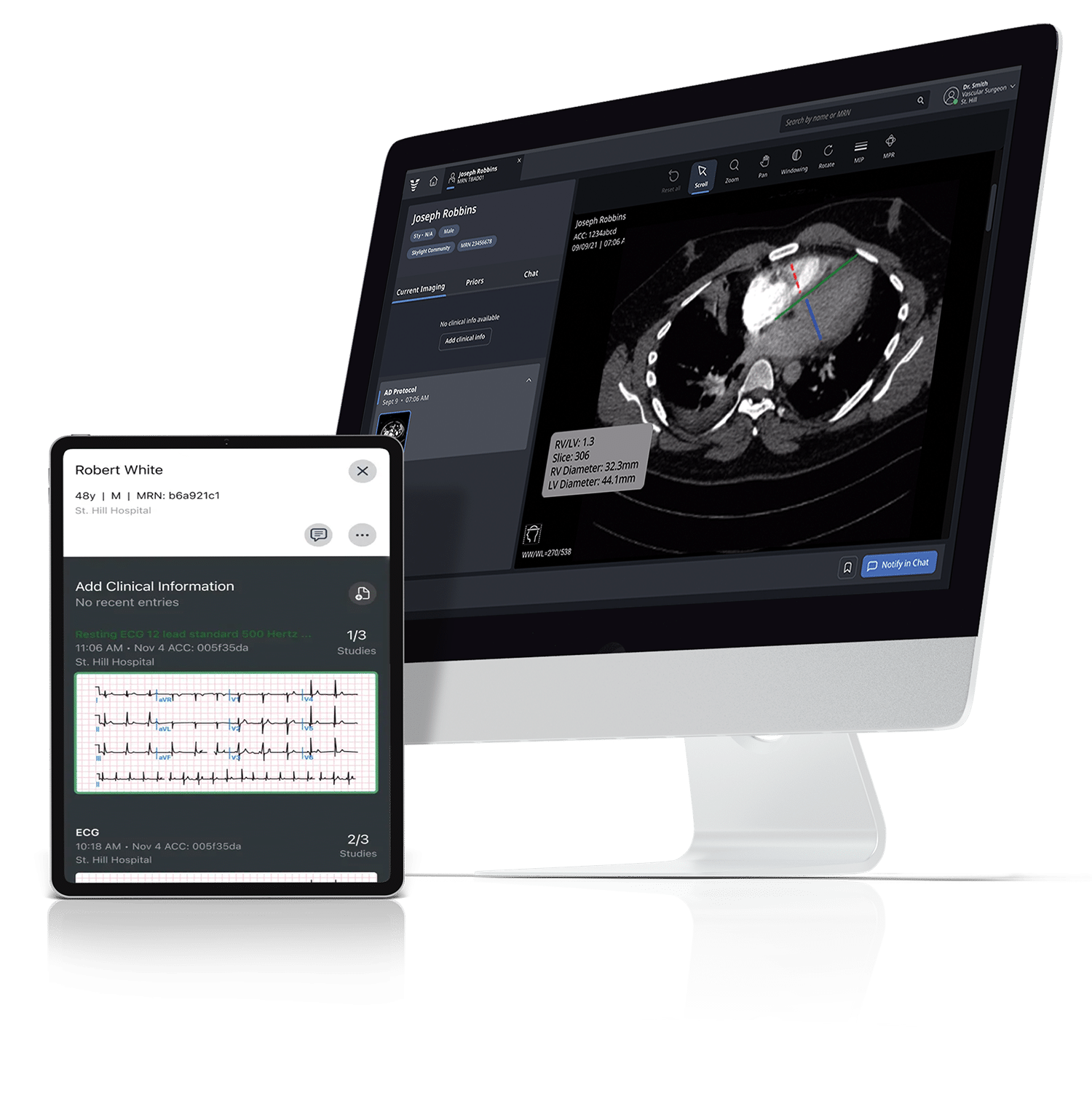
With Viz.ai, that gap is closed. The neurologist simply clicks “Cardiac Management” in the Viz Connect app to initiate an immediate consultation. Within seconds, they can enter key case details, receive referral confirmation, and begin secure, HIPAA-compliant communication with the cardiology team—without leaving the platform.
The cardiologist quickly reviews patient images and refers them for the appropriate intervention in the app: cardiac monitoring includes (1) either an external event monitor (EM) or an implantable loop recorder (ILR) to look for AFib, (2) evaluation for ablation of rapid, symptomatic AFib, (3) management of patent foramen ovale (PFO), or (4) LAAC in patients with AFib who are unable or unwilling to take anticoagulation. LAAC involves closing a small sac in the wall of the left atrium where 90% of AFib-blood clots form. LAAC prevents these clots from entering the bloodstream and causing another stroke.3 PFO is a hole in the heart that can lead to stroke as well; closure in “attributable patients” may also prevent another stroke.4
Meeting the Need for Cryptogenic Stroke Workflow at Community Hospitals
The need for an AI-powered care coordination solution, such as Viz Connect, is especially pronounced at community hospitals. The DiVERT study evaluated over 7,600 stroke patients across 12 hospitals in the United States, finding that only 5% of cryptogenic strokes at the community hospitals received cardiac monitoring versus >75% at academic centers.2 Academic sites were twice as likely to consult cardiology than community centers (34% versus 16%).2 Subsequent research, phase II of DiVERT is currently evaluating guideline-oriented neuro-cardiac workflows to reduce this heterogeneity.
Besides neuro-cardiac care heterogeneity at academic versus community hospitals, there also appears to be neuro-cardiac care disparities among genders. In a retrospective analysis of 2,699 patients from DiVERT at all sites, women were found to receive fewer Cardiology referrals (12.8% versus 15.5% for men) and less cardiac monitoring (19.9% versus 23%) after stroke hospitalization.5 The mean hospital stay was also shorter for women than men (6.8 versus 7.7 days).5 Phase II of DiVERT is also currently evaluating guideline-oriented neuro-cardiac workflows to reduce this sex disparity.
Better Outcomes with More Patients on Cardiac Monitoring and Guideline-directed Treatment
Use of Viz Connect gives cardiologists the opportunity to discuss cardiac monitoring options with their patients and treating neurology/internal medicine team while the patient is still in the hospital post-stroke. Those patients may elect to receive monitoring via ILR or EM right away to give them peace of mind that they will continue to be monitored soon after discharge. It also obviates the need for them to arrange a second hospital visit for an ILR placement, which may require an additional insurance approval, incur out-of-pocket expenses, necessitate time off work, and involve finding childcare. Unfortunately, if the delay is long, they may have a stroke waiting in the meantime for outpatient follow-up.
A study at two University of California San Diego (UCSD) comprehensive stroke centers evaluated the impact of Viz Connect on communications between their stroke neurology and cardiac electrophysiology (EP) teams and its effect on monitoring device placement.7 Before the introduction of Viz Connect, the UCSD stroke clinicians sent consultation requests to the EP team through the patient’s electronic medical record and followed up with chat messages and direct texting or calling, as necessary. Using Viz Connect, the clinicians could notify the EP team of the patient’s need for cardiac monitoring directly, obtain an almost immediate response (about 4 minutes for the consultant to view the request and 6 minutes to respond), and, if an ILR was requested, receive confirmation when it had been placed.7/
Adoption of Viz Connect resulted in an improved operational workflow and increased inpatient use of both EM and ILR devices. Inpatient ILR placements increased from 3 pre-Viz Connect to 51 post-Viz Connect and outpatient placements increased from 5 to 16.6 ILRs were also placed significantly faster; the order-to-activation time was 1 day with Viz Connect compared to 32 days without.6 Time savings were also significant for inpatient EMs (2.5 days with Viz Connect versus 13 days without).6
In another study, UCSD investigated the impact of using Viz.ai AI-powered care coordination to enhance PFO management for its patients with cryptogenic stroke. The Viz.ai PFO module allowed the neurology team to make direct referrals to the interventional cardiology (IC) team through its HIPAA-compliant app, enabling more streamlined and efficient communication between the teams. It also provided the IC team with immediate access to critical information about the patient’s PFO and any co-morbidities they may have, permitting faster evaluation. Adoption of Viz.ai PFO resulted in a 492% increase in PFO referrals, from 11 to 65 patients, and a 186% increase in PFO closures.7
Efficiencies and Economic Value with Better Care of Cryptogenic Stroke Patients
Viz Connect provides an incremental increase in revenue for hospitals by facilitating additional follow-up care for cryptogenic stroke patients before they are discharged. Those patients are also more likely to follow up and stay in the health system longer and undergo secondary procedures – such as PFO closure, left atrial appendage closure (LAAC) or ablation – to reduce their risk of having another stroke. The average healthcare cost of stroke per person, including inpatient care, rehabilitation, and follow-up care, is estimated at $140,048 in the United States.15 By expediting communication, Viz Connect reduces the time providers spend on non-clinical tasks, preserves valuable clinical resources, and helps prevent patients from being lost to follow-up – ultimately improving adherence and optimizing the patient journey.
To use a more detailed example, if a cryptogenic stroke patient receives an ILR during their inpatient visit, their case transfers from a medical to a surgical diagnostic-related group (DRG), resulting in approximately $5,000 in additional stroke reimbursement.8 By establishing a new pathway for patient management, Viz Connect improves the transition between inpatient and outpatient care. It also keeps the patient within the system longer – resulting in more office, outpatient hospital, and ambulatory surgery center visits, and on average, an additional $4,000-$8,000 of revenue.8 Furthermore, appropriate, evidence-based neuro-cardiac procedures also rise in volume, whether it be an ablation, PFO closure or LAA closure, which can result in about $30,000 of revenue.7
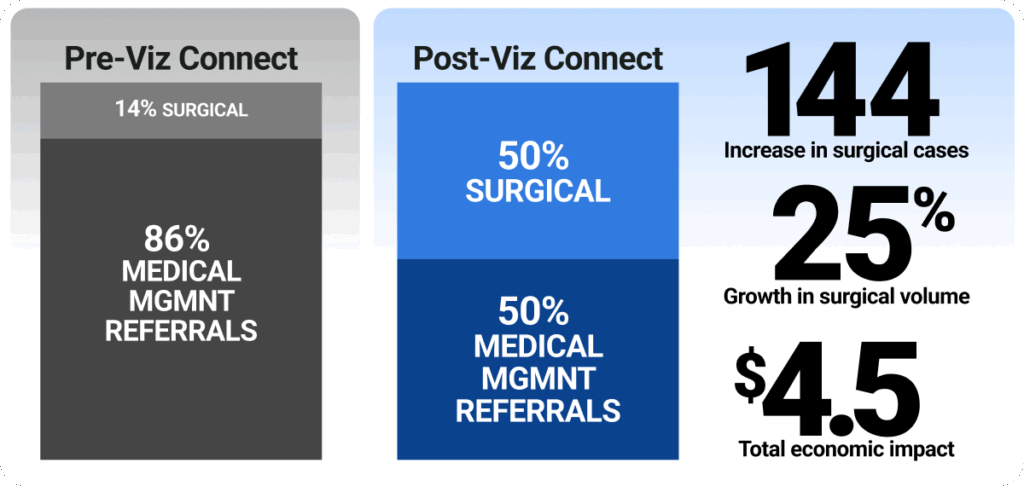
Consider a hospital with 1,000 stroke cases per year, 40% of which are cryptogenic. Pre-Viz Connect, those cases would typically be 86% medical management referrals and 14% surgical. One year post-Viz Connect, those cases will be approximately 50% medical management and 50% surgical/procedural management referrals. That translates into an incremental increase of 144 surgical cases or a 257% growth in surgical volume with a total economic impact of $4.3 million, and in appropriately selected cases, help reduce the risk of secondary stroke.13
Conclusion
Viz Connect facilitates more direct, efficient communication between care teams helping to prevent cryptogenic stroke patients from having a second stroke while delivering better clinical and economic outcomes. As the expression says, “A rising tide lifts all boats.” This format will continue to disrupt current antiquated siloed communication tools, refine and streamline “Shared Decision-Making” (SDM) processes and tailor patient-specific treatment plans for direct Neuro-Cardio Program (NCP) pathways in a secure, ethically-guided manner.14 This is particularly critical for cryptogenic patients, who often fall through the cracks due to fragmented care and variability in post-stroke cardiac evaluations. Moreover, identifying the cause of their stroke leads to removal from the “cryptogenic” group and into an actual etiology, providing a sense of relief that they know what the cause of their stroke finally was. Experts predict that this protocolized pathways in centers with dedicated NCP teams should increase protocol efficiency and reduce patient wait-times for ILR; with more AF detected, fewer strokes may result as more patients receive anticoagulation or LAAC; and PFO will be closed in a more streamlined manner in appropriately selected patients.14
References
1. American Stroke Association. Cryptogenic Stroke or Stroke of Unknown Cause https://www.stroke.org/en/about-stroke/types-of-stroke/cryptogenic-stroke
2. Rose DZ, Shah RA, Snavely J, Hairston M, Adams S, Ziegler PD, Rosemas SC, Chandler M, Carta R, Neisen KB, Franco NC, Devlin TG. Academic and Community Hospitals differ in stroke subtype classification and cardiac monitoring: the DiVERT multi-center cohort study. Front Neurol. 2024 Dec 4;15:1428731. doi: 10.3389/fneur.2024.1428731. PMID: 39697436; PMCID: PMC11652527.
3. American Stroke Association. What’s at the Heart of my Cryptogenic Stroke? https://www.stroke.org/en/-/media/Stroke-Files/Cryptogenic-Patient-Facing-Resources/A-Patient-Guide-to-Understanding-Strokes-of-Unknown-Cause-PDF-ucm477655.pdf?sc_lang=en
4. Imtiaz, Komal et al. The Incidence of Atrial Fibrillation After Percutaneous Patent Foramen Ovale Closure Detected by Implantable Loop Recorders. Journal of the Society for Cardiovascular Angiography & Interventions, Volume 3, Issue 7, 101930.
5. Cardiology Today. Cardiology consult, poststroke monitoring less common among women vs. men. February 12, 2025. https://www.healio.com/news/cardiology/20250212/cardiology-consult-poststroke-monitoring-less-common-among-women-vs-men
6. Mortin M, Shifflett B, Meyer DM, Hailey L, Yoakum S, Hsu JC, Meyer BC. CONNECT: Coordinating Options for Neurovascular Patients Needing Electrophysiology Consults and Treatments. Neurohospitalist. 2024 Sep 29:19418744241289973. doi: 10.1177/19418744241289973. Epub ahead of print. PMID: 39544275; PMCID: PMC11559453.
7. Pirahanchi, Yasaman et al. PFO-ACCESS: Augmenting Communications for Medical Care or Closure in the Evaluation of Patients With Stroke With Cardiac Shunts. Stroke: Vascular and Interventional Neurology. Volume 5, Issue 2, March 2025. doi.org/10.1161/SVIN.124.001707.
8. Based on CMS Reimbursement rates 2024.
9. McCarthy PM, et al. Surgery and Catheter Ablation for Atrial Fibrillation: History, Current Practice, and Future Directions. J Clin Med. 2021 Dec 31;11(1):210. doi: 10.3390/jcm11010210.
10. Al-Kaisey AM, et al. Atrial Fibrillation Catheter Ablation vs Medical Therapy and Psychological Distress: A Randomized Clinical Trial. JAMA. 2023 Sep 12;330(10):925-933. doi: 10.1001/jama.2023.14685.
11. Sposato LA, et al. Patent Foramen Ovale Management for Secondary Stroke Prevention: State-of-the-Art Appraisal of Current Evidence. Stroke. 2024;55:236–247. / https://doi.org/10.1161/STROKEAHA.123.040546
12. Saygi S. Atrial Fibrillation and the Role of LAA in Pathophysiology and Clinical Outcomes? J Atr Fibrillation. 2012 Oct 6;5(3):480. doi: 10.4022/jafib.480.
13. This modeling is based on Viz internal data, Medicare data and other data sources.
14. Saini H, Rose DZ. The Ghost in the Machine: Artificial Intelligence in Neurocardiology Will Advance Stroke Care. Neurohospitalist. 2024 Oct 4:19418744241288887. doi: 10.1177/19418744241288887. Epub ahead of print. PMID: 39544272; PMCID: PMC11559459.
15. U.S. National Library of Medicine. (2021, July 15). Economic burden of stroke disease: A systematic review. https://pmc.ncbi.nlm.nih.gov/articles/PMC8307880/