Team Viz
Apr 23, 2024
In a span of years—months, really—artificial intelligence (AI) has matured mightily in the public’s eye. Once met with skepticism and doubt, the world has now seen what algorithms can do (especially in healthcare).
That is, we’ve seen machines scan hundreds of X-rays with near-perfect sensitivity, detect rare diseases that went years undiagnosed, and flag concerns like Alzheimer’s before symptoms even present.
As these and other diagnostic AI applications show real-world impact for patients, healthcare stakeholders feel more comfortable embracing the technology—from patients and providers to drug companies too. Consequently, algorithms are quickly becoming an important part of care delivery.
In a recent article for the World Economic Forum (WEF), the CEO of Hackensack Meridian Health, Robert Garrett, said so, exploring the potential for AI to improve quality, outcomes, and equity. His insights join other pieces from the WEF that reflect the organization’s focus on automation, including a 60-page report on how digital transformation in healthcare can deliver more value.
As Garrett said, the technology comes at an important juncture in which disease prevalence is growing with the number of patients exceeding the providers who can see them. So what does that mean for AI’s influence and impact in the years ahead?
Here’s what experts predict:
Diagnostic AI: Doing More With Fewer Resources
Healthcare worker bandwidth is stretched and in short supply, with a projected shortage of roughly 140,000 full-time physicians by 2036. But that’s not the only constraint—costs are too, which in some cases are outpacing payer reimbursement.
Often, these concerns disproportionately hit marginalized or underserved communities. People of color tend to have longer wait times to see providers, for example. Minorities are also more likely to experience the effects of hospital revenue challenges.
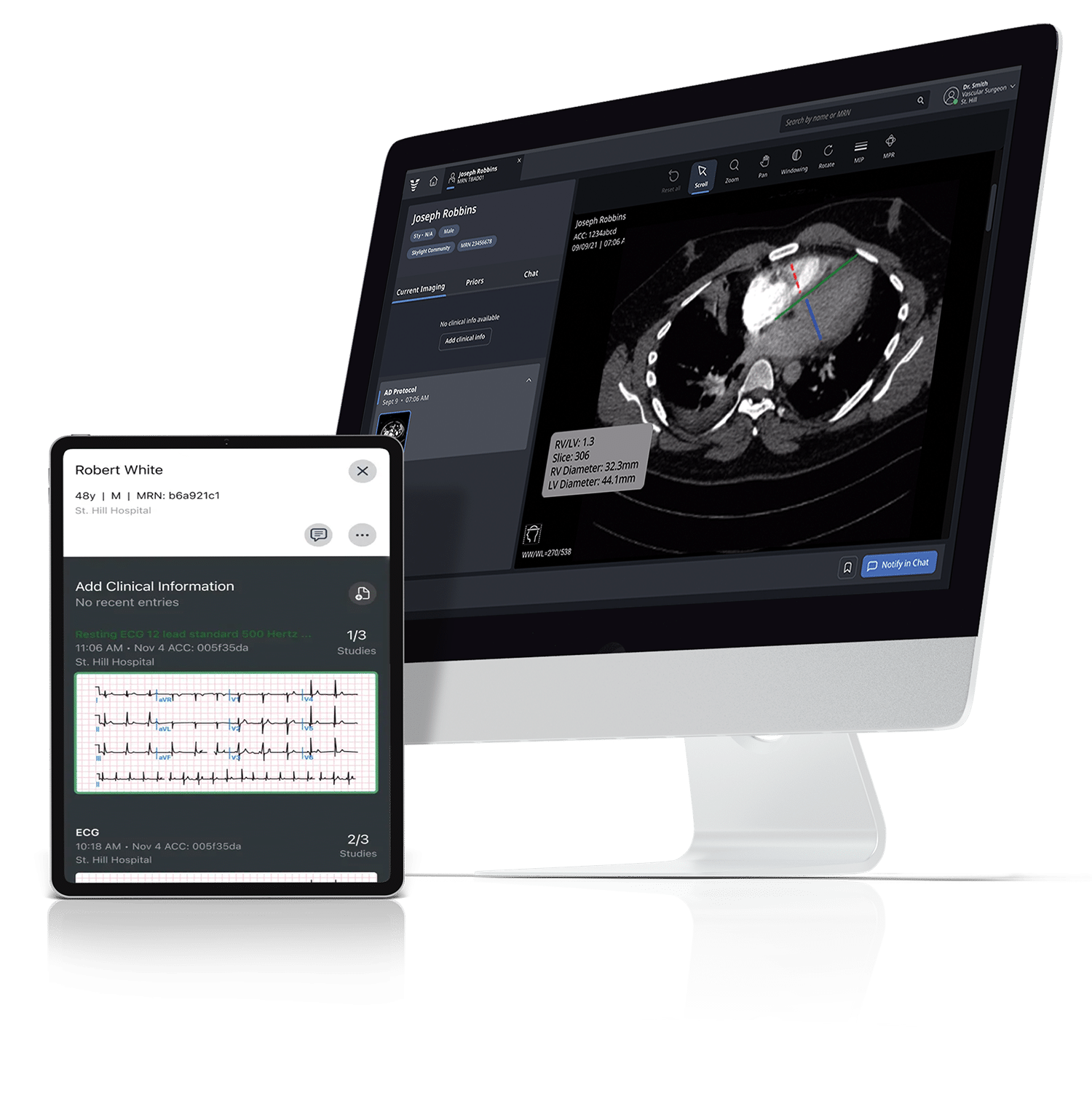
Now and in the future, diagnostic AI could help address those constraints by automating tasks, identifying clinical patterns, and recommending care plans such as labs, imaging, or medications to busy clinicians. This new genre of decision support could even help elevate the role of nurse practitioners and other nonphysician staff—something particularly beneficial for rural markets that see specialist shortages.
Shifting the Dynamics of Disease Prevalence
Diagnostic AI isn’t just filling in the gaps of an under-resourced healthcare system—it’s also advancing the system itself through preventive and early-stage care.
That shift comes as people live longer overall but also spend more time in bad health, the WEF reports. From 2000 to 2019, for example, Americans spent 1.5 more years in a state of illness as the prevalence of conditions such as obesity, heart disease, diabetes, cancer, and Alzheimer’s have increased. And yet, these known and diagnosed conditions are just the tip of the iceberg: An estimated 100 million people live with undiagnosed chronic diseases.
While an aging population can contribute to those statistics, it’s not just a product of Baby Boomers and their sizeable cohort. Factors like lifestyles and access to care are all part of the calculus of what’s been called the “U.S. health disadvantage.” Costs matter too, of course: Roughly a quarter of people delay care because of how much that care costs. That, in turn, can worsen poor health.
AI, however, has the potential to shift the dynamics of disease prevalence for a more seamless patient journey. Experts suggest algorithmic-enabled care could identify problems not just in early, more treatable, and less costly stages—as we’ve seen with hypertrophic cardiomyopathy (HCM)—but also recognize patterns that otherwise would have gone undiagnosed.
Overcoming Bias With Purpose and Partnership
Bias is a common criticism of AI in healthcare, and rightly so: In his WEF article, for example, Hackensack’s Garrett points to algorithms that were modeled from light-skinned people that missed diagnoses for people of color.
This emphasizes the importance of building algorithms with more intention and purpose, which should remain a future priority for all healthcare innovators. At Viz.ai, we’re strong believers in equitable AI: We use diverse patient data across age, sex, and race so that our algorithms are designed to help avoid bias.
But of course, AI and healthcare intersect at a complex and evolving place. Creating an ethical, effective, and efficient AI solution isn’t something any one organization can do alone. Garrett mentions the importance of partnership in his WEF article, something we’re committed to as well: We’ve developed relationships with pharma to expand the library of diagnostic algorithms across multiple therapeutic areas—and we’re looking for even more pharma partners so that we can do more, together.
All Eyes on AI in Healthcare, Today and Tomorrow
Diagnostic AI comes at a challenging but exciting moment for the healthcare continuum. As resources contract and diseases go undetected, the promises of automation are already here, readily supporting clinicians, patients, and pharma stakeholders.
But there’s a lot more innovation up ahead, and through the power of partnership, we’re excited to be a part of it. By working across in-demand therapeutic areas in cardiology, memory care, oncology, and beyond, we aim to improve patient experiences, equity, and access so that no patient gets missed.
If you’re a life science company interested in working together to develop an AI-driven program to accelerate patient diagnosis and treatment for your therapy or device, reach out to see how we can help.