Team Viz
May 16, 2023
5 min
Radiologists’ workloads have increased dramatically over the past several years both during regular working hours and when on call. This is due in part to the growing use of CT scans by emergency room physicians who must rapidly diagnose and triage patients, many of whom need urgent care.
One study at a large tertiary academic medical center showed that the number of CT studies during on-call hours, measured in relative value units (RVUs), increased by 52% between 2012 and 2019, while the comparable number of emergency room visits grew by just 23%. During that period, RVUs for the most common CT exams increased significantly – brain CT exams were up 33%, abdominal CTs grew 70%, thoracic-lumbar spine CTs were up 1,375% and head and neck CTAs by 287%.
CTs are an invaluable diagnostic tool but growth of this magnitude puts existing systems and staff under enormous pressure as they try to manage much larger workloads and sustain high quality reviews to ensure diagnostic accuracy and patient safety. It is no surprise that radiologists facing these stressors on a regular basis are experiencing work frustration and burnout.
It seems almost inevitable that asking radiologists to keep reviewing growing volumes of studies, faster, on longer shifts will at some point lead to a decrease in interpretive accuracy.
But a recent review revealed that there is currently insufficient evidence to determine scientifically what the appropriate workload, speed, or duty hours for radiologists should be. That said, while researchers try to determine how radiologist workload or duty hours correlate to review accuracy, these busy professionals clearly need help alleviating some of this burden.
How Can Radiology AI Software Help?
Artificial intelligence (AI-) based prioritization software, also known as computer-aided triage and notification (CADt) devices, can analyze patients’ radiology images, and arrange cases in priority order in the radiologist’s reading queue based on the time sensitivity of the findings. This helps to increase the likelihood that time-critical diseases such as large vessel occlusion and intracranial hemorrhage, are diagnosed and treated quickly. CADt devices help to optimize the radiologist’s time and attention and make best use of a stretched resource.
Communicating Incidental Findings
Often during an imaging review, a radiologist will spot actionable incidental findings (AIFs), which are unrelated to the clinical indication for which the imaging test was ordered but still require follow up. As the use of imaging in emergency departments has increased, so has the number of patients with AIFs, and it has become challenging to track them, especially in large health systems. If AIFs are not properly communicated and followed up, not only could it jeopardize the patient’s health, but it could also incur additional costs for the patient and health system and increase the likelihood of a lawsuit. As a result, many health systems have implemented methods of tracking AIFs. One example involved the use of a closed-loop AIF program within the emergency department of 11 satellite hospitals of a large academic health system. Radiologists reported AIFs through system macros and a standardized form integrated into the dictation software. When the form was completed, it triggered an email to be sent to a dedicated nurse navigator who documented the findings and coordinated follow-up imaging or clinic visits with patients, primary care providers, and specialists. A total of 1,207 AIFs were submitted to the new workflow between July 2021 and May 2022, including at least 10 new cancers.
Following Up on Referrals
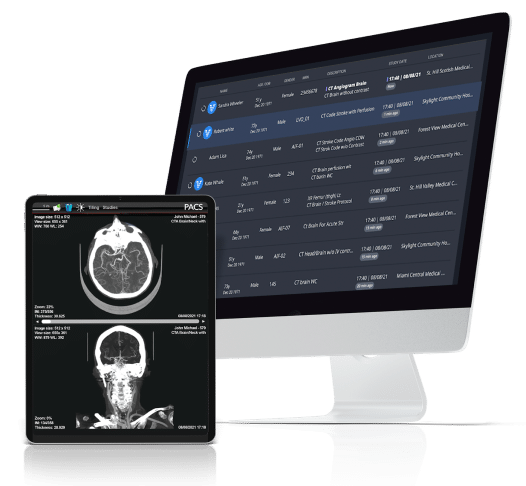
However, some clinically necessary follow-up imaging does not occur and a retrospective study at an academic health system sought to determine reasons why that happens. Researchers used an automated communication and tracking tool embedded in the Picture Archiving and Communication System (PACS) and electronic health records to monitor progress. Out of the study sample of 5,856 follow-up imaging recommendations, 4,881 of them were flagged as clinically necessary. If imaging did not occur within one month of the requested completion date, the tool prompted a safety net team to reach out. Follow-up imaging was completed for 74.8% of the clinically necessary referrals. Several factors reduced the likelihood that a patient would have that important follow-up imaging. They included living in a socioeconomically disadvantaged neighborhood, being in an inpatient or emergency department care setting, and the referrer having a surgical specialty.
Improving Communications
Communication is recognized as one of the biggest pain points for radiologists. Dr. Kevin Abrams, Chief of Radiology and Director of Neuroradiology at Baptist Hospital and Health Systems, describes in the webinar entitled “AI for Radiology. Nothing Artificial About That” how he uses AI in radiology, specifically the web and mobile apps from the Viz™ Radiology Suite, to review imaging, improve team communication, and enhance patient care coordination.
Dr. Abrams has Viz AI-powered alerts set up for large vessel occlusion (LVO), intracerebral hemorrhage (ICH), pulmonary embolism, aortic dissection, and aneurysm. If the Viz platform detects an LVO, for example, it will send him an alert with a tagged image of the exact CT slice that shows the suspected occlusion for his review. If, after reviewing the high-fidelity 3D image, Dr. Abrams confirms the diagnosis, he will send the patient’s information to his entire urgent care team simultaneously in real time. Then, Viz group texting ensues, as they coordinate the patient’s care across the neuroradiology, neurology, nursing, and neurointerventional radiology departments.
Dr Abrams commends the virtues of the Viz chat function, noting it is “full stack, secure communication, HIPPA-compliant, encrypted, so the whole team could be on the same page on the same patient communicating in parallel rather than in serial fashion.”
He noted that in the past, he would have had to make a phone call to the neurologist to give them the results. Then, if they were not available, wait for them to call back. Now over 90% of their cases are done through the Viz chat function.
Parallel communication, facilitated by the Viz platform, both expedites and improves patient care. Dr. Abrams referenced a UC Davis study in which the Viz.ai platform was implemented in a comprehensive stroke center and network. Researchers analyzed 82 neurointerventional cases pre vs post time periods and reported a reduction in patient door-to-groin time for thrombectomy from 157 minutes to 95 minutes, a 39% improvement, with the Viz.ai platform. This advance was enabled by the Viz platform providing immediate access to patient imaging and facilitating streamlined communications across the multidisciplinary care team. This time saving is a huge advantage for stroke patients for whom time is brain and where every minute saved facilitates their recovery.
If you’d like to learn more about the triage and communications advantages of our radiology AI software or enterprise AI, visit our platform page or get in contact with us by filling out the form below.