Team Viz
Sep 01, 2021
5 min
Viz.ai is expanding into cardiovascular disease to address the vulnerabilities in coordinating care in pulmonary embolism and aortic disease
The World Health Organization recently published a study showing that the number of people living with hypertension has doubled to 1.28 billion since 19901. More than half of this group – close to 720 million people, are not receiving the treatment that they need. High blood pressure is an important risk factor for heart failure, atrial fibrillation, chronic kidney disease, heart valve diseases, aortic syndromes, and dementia, in addition to coronary heart disease and stroke.
The founding of Viz.ai created a new category of Intelligent Care Coordination. Intelligent Care Coordination focuses on increasing access to care by connecting the right patient to the right doctor at the right time. The first artificially-intelligent product that was produced by Viz.ai uses machine learning to identify and triage suspected strokes minutes after the head scan has been completed. Clinical studies have shown that Viz LVO has decreased length of stay, increased access to care, and improved clinical outcomes for patients after implementation2,3.
Viz.ai began in stroke because it was a challenging pathology rife with barriers to making critical, time-sensitive decisions. Viz.ai transformed the serial process of patient intake into a parallel, synchronized process using the Viz Mobile App. Now, Viz.ai is expanding into cardiovascular disease to address the vulnerabilities in coordinating care in pulmonary embolism and aortic disease.
What challenges exist in vascular care coordination today?
Lack of Clear Communication & Patient Information
Interventionalists typically receive patient information piecemeal and over the phone. Specialists report they are often speaking to someone on the phone at an outside ED who is not familiar with the pathology and urgency of the disease, making it harder to triage from a distance. Vascular Surgeons and Interventional Radiologists also report that access to imaging from outside hospitals is extremely difficult. Hospitals within the same system may have different configurations that make it challenging to share and read patient scans. Often, patients are transferred via ambulance to the treating hospital with CD-ROMS of their scans taped to their chest. The lack of a cloud-based image sharing service creates challenges for patient triage. In the best of cases, physicians use Facetime calls with the local care teams in order to assess the patient remotely prior to transfer.
Delays in Care
Aortic repair is an image-dependent operation. In order to adequately prepare for the procedure, vascular surgeons and interventional radiologists must have a good understanding of several variables, including the patient’s aortic morphology, access vessel sizing, comorbidities, landing zone, aortic neck. Without imaging, it’s impossible to prepare for an efficient procedure. In addition to this, aortic endovascular repair often requires mission-critical medical devices. Preparing the necessary devices can require calling multiple device reps and coordinating the delivery and receipt of stent grafts, sheaths, catheters, wires, and balloons for the procedure.
Unnecessary Costs
When an aortic emergency is called in by an outside hospital without imaging or a workup, the on-call vascular surgeon must make a decision to either activate the team just in case an intervention is required, or wait and see. False team activations can result in mounting hospital costs and burnout for care team members. These costly and time-consuming false team activations can be prevented with access to AI-powered alerts and imaging. While patients can present directly to the comprehensive center, there are many cases in which patients present to outside hospitals and must be transferred. The lack of a unified image transfer can often result in patients being re-imaged upon arrival to the treatment center. The process of re-imaging patients can further delay care. Finally, there are cases where if interventionalists had access to imaging prior to accepting transfer, they could save futile end of life trips instead of providing palliative care for the patient and keeping them closer to their family. This is especially common for aortic rupture and dissection patients.
Applying the progress made in stroke to new areas of acute need
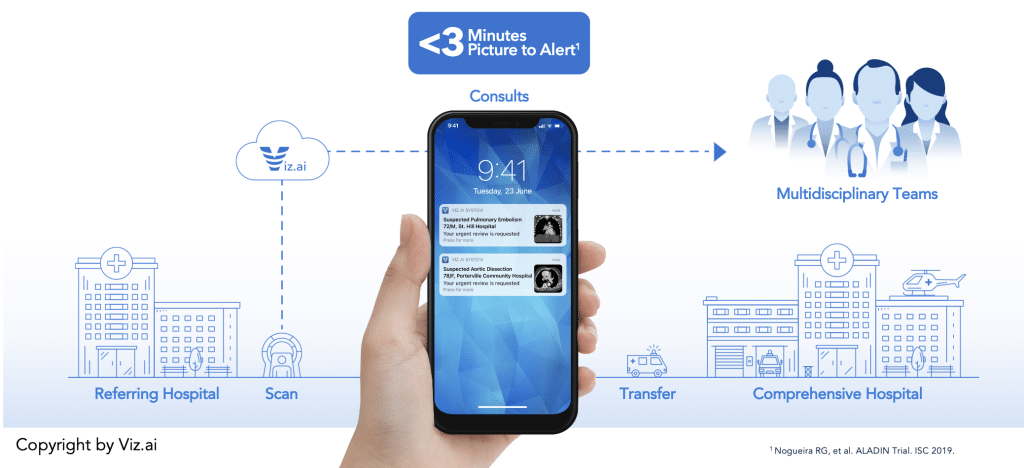
With Viz, every member of the on-call medical team is automatically alerted to suspected disease in their hub and spoke network within minutes.
- Healthcare Data: Viz.ai ingests data from any imaging modality (X-Ray, CT Angiogram, Magnetic Resonance, etc.
- AI Analysis: The Viz.ai cloud-based AI algorithms automatically detect suspected disease
- Trigger Action: Viz.ai connects patients to doctors as well as doctors to doctors
- Therapy Enablement: The use of Viz.ai results in improved clinical outcomes and has shown an increase in urgent procedures such as mechanical thrombectomy
The results are simple: patients who are treated faster have better outcomes. The progress made in stroke can be translated to acute vascular disease.
Using AI to remove barriers to efficient vascular care
Viz PE is a brand new, AI-powered module that facilitates efficient care coordination for suspected pulmonary embolism disease. Viz.ai uses machine learning to search the pulmonary arteries for the presence of emboli. Once a pulmonary embolism is detected, the on-call members of the care team are automatically alerted and provided with imaging and a complete, up-to-date clinical view of the patient. The purpose of the Viz PE app is to enhance a PE response team’s workflow.
Not every pulmonary embolism requires urgent intervention. Viz PE is customizable, and can be configured so that the desired members of the PE response team can be notified prior to the rest of the PERT team, thereby serving as a failsafe for false activations. If the patient requires multidisciplinary care, their record can be easily shared with relevant members of the interventional team within the Viz PE app. This progressive team activation can be used to effectively match the urgency with the acuity of the patient.
The AI-powered alert includes access to patient imaging, labs, a directory of on-call and off-call team members across the hospital network, and a HIPAA-compliant patient communication feature. Viz.ai can also be used to facilitate patient enrollment in clinical trials based on predefined criteria.
Viz Aortic was created to find and triage acute aortic pathology across health systems and geographies. The machine-learning algorithm automatically searches CT scans for markers of Type A and Type B aortic dissections. The module reads through the CTA starting from the aortic root to the iliac bifurcation. The sensitivity and specificity of the algorithm is highly powerful, with scores greater than 98%. Once this acute pathology is detected, the designated members of the aortic care team are notified on the app with the suspected pathology, patient status, and comprehensive imaging studies.
Key takeaways
- Viz.ai uses deep learning to find suspected vascular disease and alert the on-call interventional vascular team across hospital networks
- The module saves time and reduces effort in image acquisition for case planning
- The Viz.ai mobile app allows for for identification of both emergent and incidental pathologies
- Having earlier access to imaging will intuitively improve the overall aortic workflow
References:
- Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1,201 population-representative studies with 104 million participants’ by the NCD Risk Factor Collaboration (NCD-RisC) is published in The Lancet. DOI: 10.1016/S0140-6736(21)01330-1
- Hassan AE, Ringheanu VM, Rabah RR, Preston L, Tekle WG, Qureshi AI. Early experience utilizing artificial intelligence shows significant reduction in transfer times and length of stay in a hub and spoke model. Interv Neuroradiol. 2020;26(5):615-622.
- Morey JR, Fiano E, Yaeger KA, Zhang X, Fifi JT. Impact of Viz Lvo on Time-to-Treatment and Clinical Outcomes in Large Vessel Occlusion Stroke Patients Presenting to Primary Stroke Centers. Neurology; 2020.
