Team Viz
Jan 30, 2026
By Andrew M. Ibrahim MD, MSc, Chief Clinical Officer at Viz.ai and
George D. Zuidema Professor, University of Michigan
Much of my academic career has been spent working with rural hospitals to understand how care is delivered on the ground. That work began with a study I presented at the National Rural Health Association meeting in 2016, and it has continued over a decade with our most recent work featured at the 2025 meeting.
Despite all the challenges facing rural hospitals, they do a number of things exceptionally well. In our studies including millions of Medicare beneficiaries, we found that critical access hospitals perform common surgical procedures safely with the same or better outcomes than their urban peers. Moreover, we found they do it at lower costs than their urban peers. Finally, when given the opportunity, many patients in rural communities prefer to have their care closer to home.
The challenges that persist tend to show up at the boundaries of care, where speed, coordination, and access to external expertise matter most such as strokes or heart attacks.
From that lens, most rural hospitals are navigating two competing demands every day. First, staying tightly connected to regional partners for time-sensitive conditions that require capabilities beyond what can reasonably be provided locally. Second, preserving the ability to care for patients locally when it is safe and appropriate, so volume, trust, and continuity are not lost unnecessarily.
Balancing those two realities is not easy, and most systems are not designed to support both at once.
When there are gaps and uncertainty persists
Gaps in care for rural communities surface most in particular conditions. Time-sensitive conditions expose how difficult it can be to quickly align imaging, specialists, and transfer decisions across distance. Stroke is often cited because it is well-studied, but the underlying challenge is broader. Many time sensitive conditions, like heart attacks, trauma accidents and large blood clots to the lung also pose similar time-sensitive challenges.
What happens when there is limited time and limited information? Patient care is uncertain and stalled. In practice, uncertainty drives transfers. And when those transfers are unnecessary the burden compounds; patients are not getting better care, the often only ambulance in the county is now tied up for hours, and patients face a new travel burden to get back home. But if we could fill that uncertainty with the right data, information sharing and decision support, we can balance the load at hospitals and get patients to the right place, at the right time, even when that means not traveling.
Addressing the Uncertainty: Where Viz.ai can be helpful
Viz.ai was built to support exactly these moments, without assuming that rural hospitals need to change who they are.
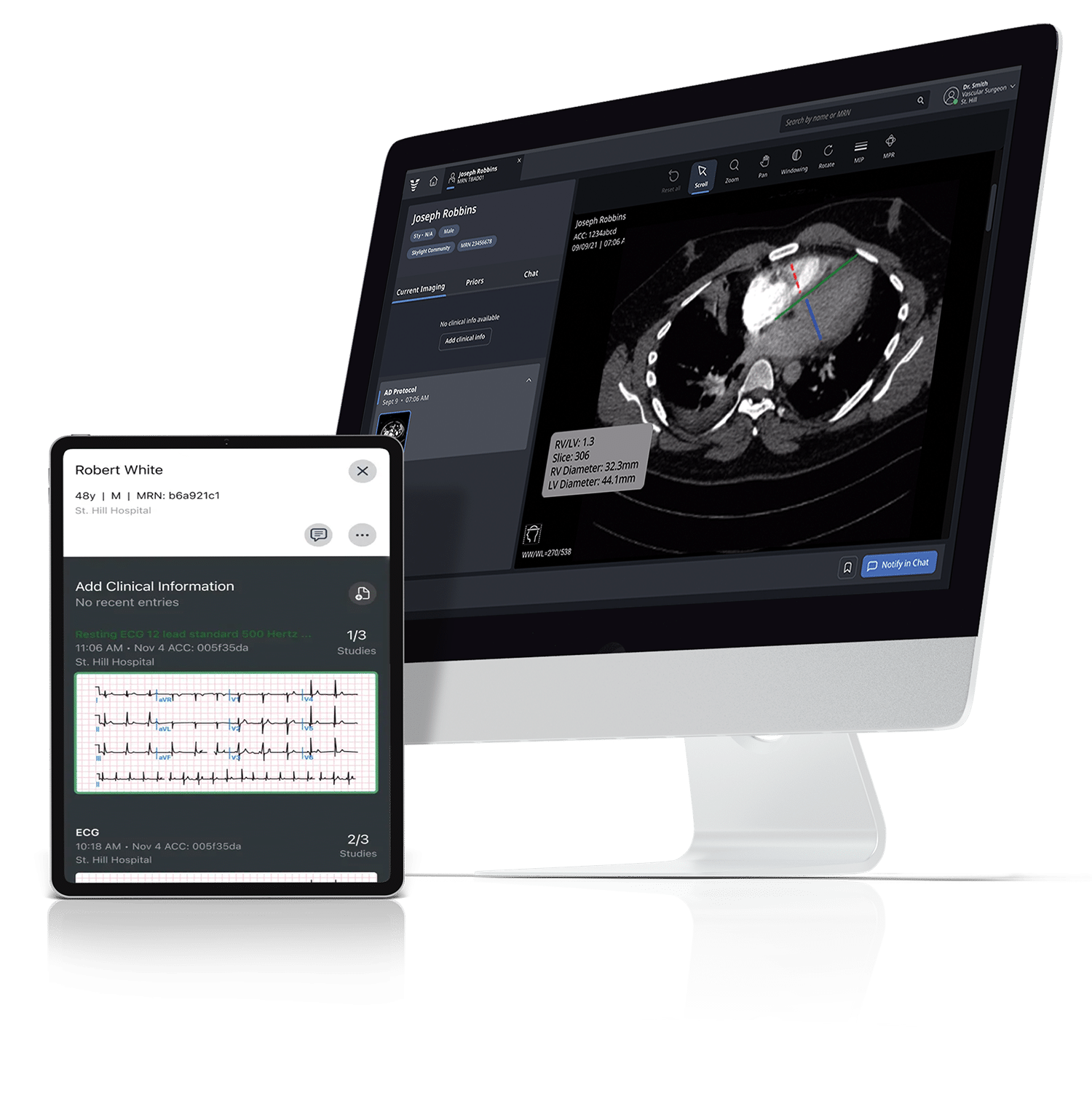
When regional escalation is needed, Viz.ai helps teams connect faster. Critical findings are surfaced early, specialists and receiving centers are aligned sooner, and transfer decisions happen with greater clarity.1
At the same time, Viz.ai supports local care. By improving access to real-time insights and shared situational awareness, it can increase confidence in decision-making and help avoid transfers driven primarily by lack of information or delayed communication.
That balance matters. Keeping care local when appropriate supports patients, families, and the long-term viability of rural hospitals. Moving patients quickly when higher-level care is needed improves outcomes. Viz.ai is designed to help with both.
Built for rural reality
Viz.ai includes FDA-cleared, guideline-supported2, and CMS-reimbursed capabilities, and has been deployed across a wide range of hospital settings, including low-volume and resource-constrained environments. About one in four of the nearly 2,000 hospitals using Viz.ai are rural, and the platform plays an important role in connecting them to their regional system. Importantly, it integrates into existing workflows and does not require new service lines or staffing models.
Connecting rural hospitals into their regional system has been a longstanding challenge. We now have the evidence3 and technology to make it a reality. To right-size care that can be done safely and locally, while also identifying patients who need higher levels of care and immediately get that information shared and transfer coordinated.
1 Sevilis, Theresa, Morgan Figurelle, Amanda Avila, Caitlyn Boyd, Lan Gao, Gregory W. Heath, Hira Ayub, and Thomas Devlin. 2023. “Validation of Artificial Intelligence to Limit Delays in Acute Stroke Treatment and Endovascular Therapy (VALIDATE).” Abstract WP81, Stroke 54
2 Dusenbury, Wendy, Claranne Mathiesen, Michelle Whaley, Opeolu Adeoye, Thabele Leslie-Mazwi, Shavonne Williams, Cesar Velasco, Samarth Shah, Nicole R. Gonzales, and A. W. Alexandrov, on behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. 2023. “Ideal Foundational Requirements for Stroke Program Development and Growth: A Scientific Statement from the American Heart Association.” Stroke 54 (4): E175–E187.
3 Rudilosso, Santiago, and Albert Song. 2022. “Artificial Intelligence Triage for Large Vessel Occlusion: Impact on Stroke Workflow and Outcomes.” Abstract 1253, Neurology 98