Viz™ AORTIC
A Review of Mature Machine Learning and Artificial Intelligence...
Background After years of both increasing enthusiasm and skepticism by surgeons and patients, the first artificial intelligence (AI) and machine...
May 05, 2023

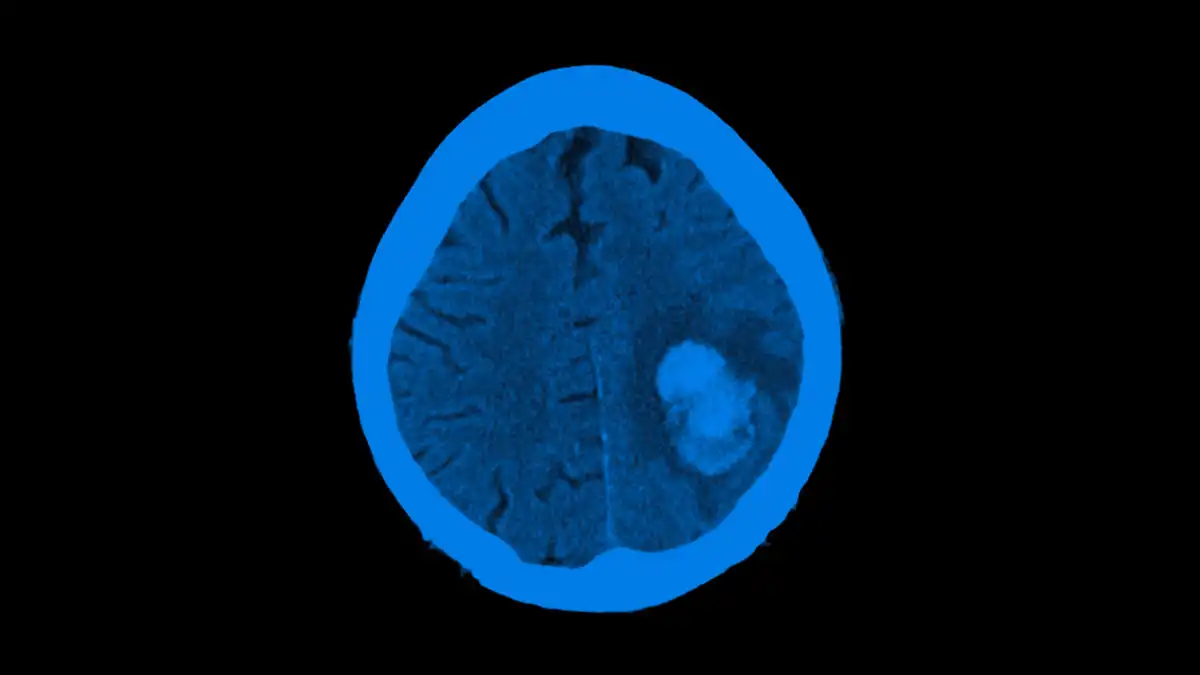
Large vessel occlusion (LVO) acute ischemic stroke is a time sensitive disease process. Technology that could shorten the time to mechanical thrombectomy (MT) holds great promise, but experience and data on these applications are sparse. We describe our initial experience with Artificial Intelligence (AI) for automated LVO detection (aLVOd) in a hub and spoke network.
This is a retrospective chart review of consecutive code stroke cases at a comprehensive stroke center and two spoke hospitals. Viz AI was implemented from May 2019 to December 2019, during which time 100 consecutive LVO alerts were evaluated. Baseline clinical characteristics were collected on all aLVO alerts and from historical LVO controls taken to the angiography suite for intervention from the 6 months prior to AI implementation. Details of medical treatment, CT/CTA interpretation by blinded Neuroradiologists (confirmed LVO, normal, or significant cerebrovascular finding without LVO), final diagnosis, results of MT, clinical outcomes, and stroke workflow metrics were collected. Categorical variables were compared with Pearson chi-squared testing and continuous variables with Wilcoxon rank sum testing.
A total of 680 code strokes were evaluated during the AI study period. The average age and NIHSS score of the 100 aLVOd patients were 69 (IQR 57, 80) and 4 (IQR 1, 13.75), respectively. There were no significant differences in baseline characteristics of LVO patients identified by aLVOd, those LVOs missed by aLVOd, or historical LVO controls undergoing MT. A total of 68 patients were diagnosed with LVO during the AI study period; 45 (66.2%) were identified by aLVOd and confirmed by neuroradiology, and 23 (33.8%) were missed by AI. The majority of LVOs missed by AI were distal M2 or posterior circulation occlusions (60.8%). Of the 100 total aLVOd alerts, 55 were not LVO based on the neuroradiologist interpretation (18 were normal, 36 high grade intracranial atherosclerosis, and one was non-diagnostic). The average NIHSS score of LVO patients detected by AI was 11 (IQR 3, 19). Forty-one patients during the AI study period underwent MT and 36 historical LVO controls underwent mechanical thrombectomy.
The sensitivity and specificity of aLVOd was 66.2% and 91% while the positive predictive value and negative predictive values of AI were 45% and 96%, respectively. Median time from CTA completion to treating team notification for all patients was significantly shorter for aLVOd patients (8 minutes (IQR 4.25, 9) v 17 min (IQR 13, 28.5), p<0.001). Door to arterial puncture was also significantly faster for patients transferred from a spoke to a hub for MT (141 minutes (IQR 128.5, 168) v 185 min (IQR 151, 241), p=0.027).
VizAI aLVOd is a robust screening tool for identifying LVO based on its high negative predictive value. This system is a valuable adjunct to traditional imaging interpretation. The use of AI to detect LVO improves stroke workflow metrics in a hub and spoke stroke system of care.
Researcher:
Dr. D Dornbos
Publication:
Journal of NeuroInterventional SurgeryDate Published: August 4, 2020
Aug 04, 2020