Team Viz
Aug 17, 2021
5 min
COVID-19 has changed hospital economics. Providers are forced to limit elective procedures and patients are foregoing care.
The COVID-19 pandemic has changed hospital economics. Providers are forced to limit elective procedures and patients are foregoing care even for emergencies as they are afraid to come to the hospital. This has left health systems with uncertainty, trying to find ways to continue providing cost effective, high quality care during an unprecedented pandemic that has made coordinating patient care that much more difficult.
As former Assistant Vice President of Neuroscience at Baptist Health South Florida and former Executive Director of Neuroscience at Piedmont, I have seen Viz play a critical role coordinating care during this crisis; reducing time to treatment, improving outcomes, increasing access to care and helping our system recover economically. By helping coordinate care through optimizing workflows, Viz helps transfer the right patients, increasing mechanical thrombectomy rates and reducing length of stay.
Technology overview
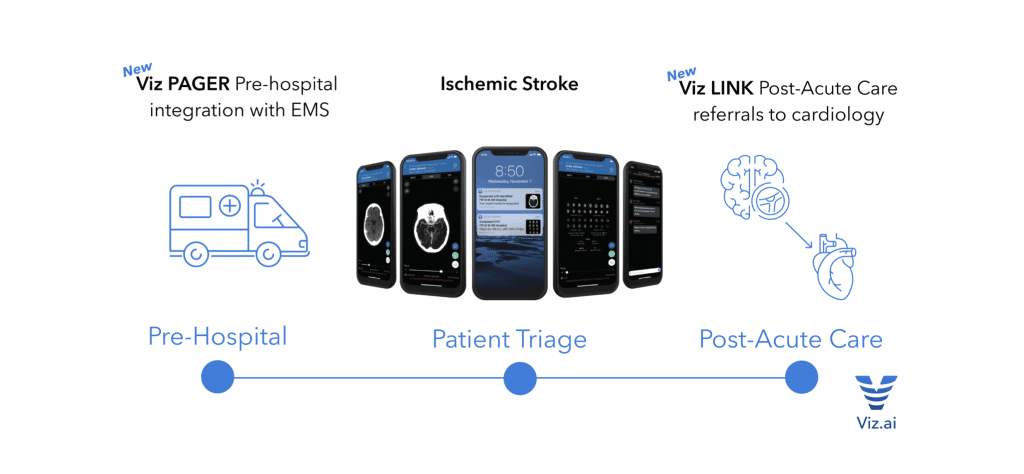
Viz utilizes proprietary artificial intelligence and deep learning technologies to automatically detect and alert clinicians to acute pathology and is paired with a PACS quality mobile image viewer and HIPAA compliant communication platform to facilitate synchronized coordination of care to stroke patients.
The ischemic stroke platform includes automated and AI driven large vessel occlusion, advanced CTP perfusion, NCCT, CTA and MRI viewing, and simplified ASPECTS scoring. Viz is also capable of integrating with EMS for pre-hospital care coordination with Viz PAGER, and post-acute care referrals for cryptogenic stroke patients directly to cardiology with Viz LINK.
In centers across the country, this technology has revolutionized how stroke patients are cared for. Prior to having Viz, stroke specialists were dependent on quick triage and communication from physicians in the emergency department to push patients to specialists. Now, the entire stroke team is alerted almost instantly, often when the patient is still in the scanner, and the stroke team pulls appropriate patients to intervention. This is a paradigm shift, from a push model to a pull model. In both standalone centers and hub and spoke models, Viz has demonstrated significant time savings by alerting treating specialists as early as possible in the workflow and enabling coordination of care sooner.
Many peer reviewed publications have found that treating patients faster improves outcomes. Associated with time savings at Valley Baptist, Dr. Ameer Hassan found significant 2.5 day and 3.5 day reductions in total hospital length of stay and neuro-ICU length of stay using Viz. At Mount Sinai, New York, these time savings have resulted in improved outcomes for patients. Drs. Fifi et al demonstrated significant improvements in 5-Day NIHSS, discharge mRS, and 90- Day mRS.
CMS Grants Viz LVO a New Technology Add-On Payment
NTAP is an acronym for New Technology Add-On Payment. NTAP recognizes that current payment rates can be a barrier to adopting new technology and is an additional payment for hospital stays that use new technology determined by CMS to provide substantial clinical improvement and where the current MS-DRG payment would be inadequate.
Viz LVO is the first A.I. medical software to receive NTAP. Viz demonstrated to CMS a significant reduction in time to treatment and improved clinical outcomes in patients suffering a stroke.
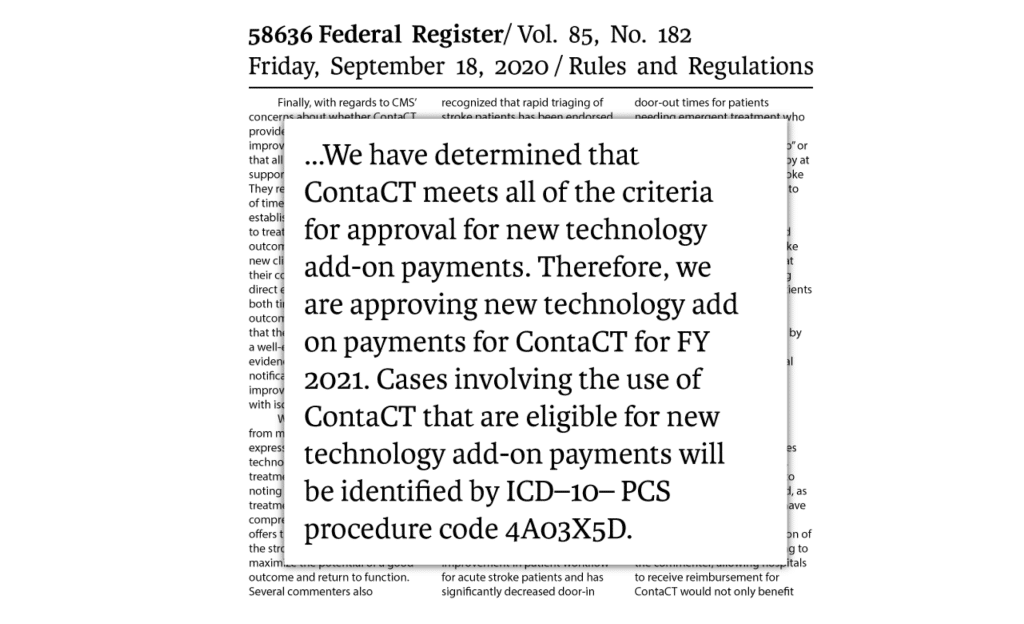
CMS has determined that $1,040 is the maximum add-on payment for each use of Viz LVO (formally Viz ContaCT). If costs exceed payments, Medicare pays the lesser of:
- 65 percent of the costs of the new technology, or
- 65 percent of the amount by which the costs of the case exceed the DRG payment for the case.
Case Study: Single Center Hospital
In a single center hospital with 500 suspected ischemic strokes per year, an estimated 131 cases will qualify for NTAP, receiving up to $1,040 per patient. This results in a total projected impact of $136,240.
Case Study: Multi-Center System
In a multi-center system with 1,500 suspected ischemic strokes per year, an estimated 394 cases will qualify for NTAP, receiving up to $1,040 per patient. This results in a total projected impact of $409,760.
Maintaining high quality and cost-effective patient care during COVID-19
Since the start of COVID, we have seen total stroke volume decrease, increased strokes in younger patients, more patients presenting with complicated or atypical strokes, and fewer neurologists in EDs helping to triage these patients. The complicated presentations and the reduced numbers of providers in spokes has challenged our ability to maintain delivery of optimal care to patients.
Viz has helped to triage these patients remotely with maintained communication across the entire care team and has proven to be critical to not only provide optimal patient care through this health crisis but to do so cost effectively.
Patient safety and resource management is of utmost importance during a pandemic. Reducing futile transfers and ensuring that only patients with large vessel occlusions that will benefit from mechanical thrombectomy are transferred to hub centers is essential. Minimizing futile transfers decreases the risk of exposure for patients transferred to hub hospitals that typically have more COVID patients and helps to reserve limited resources and ICU beds for COVID patients at the hub. Bringing patients that will benefit from thrombectomy will further assist hubs financially as the MS-DRG for intervention is much higher than for medical management.

When spokes retain patients who are unlikely to benefit from mechanical thrombectomy, they are able to manage the patient medically in the same manner they would be cared for at the comprehensive center and can bill and collect for the services they provide.
Patients with large vessel occlusions that can benefit from thrombectomy are costly for spoke hospitals when they are not transferred. These patients often have large infarcts driving long lengths of stay both in the ICU and in the hospital. These outcomes are not only suboptimal for the patient but costly for the hospital, as the costs associated with care often exceed the DRG payment received for the services provided.
Conclusion
Early notification of specialists with Viz helped us cost-effectively optimize stroke triage during COVID across a large hub and spoke network, helping to pull only the patients that are likely to benefit from mechanical thrombectomy to the comprehensive center. This helped manage resources at the comprehensive center appropriately, maximizing ICU beds and PPE, providing optimal care to patients that will benefit from thrombectomy at the hub and empowering our spokes to medically manage non-thrombectomy candidates without transfer.
